First it was the great L4-5 Disc Rebellion of 2010 and this January marked the terrifying Melanomic Insurrection of 2012. If I didn’t know better, I’d think my back is trying to kill me.
Make sure you check your moles often and get anything you find suspicious cut out ASAP.
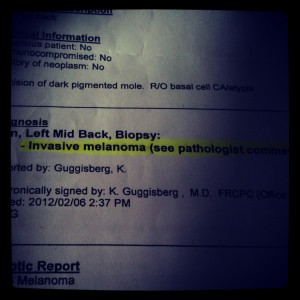
Mine was full blown Malignant Melanoma, though only Stage T1a (.79mm Breslow thickness, Clark level III, non-ulcerated, 0/mm2 mitoses, absent Angioinvasion & Neurotropism) – but a mighty scare, nevertheless. It’s out now and I have a >90% chance I’ll be ok, but you don’t seem to know its in your lymph nodes until its too late. Needless to say, I’ll be watching these other little f_ckers with an eagle eye from this point on.
Ironically, the country that probably wrecked my disc with manual labour, is also the country that most likely poisoned my mole with UV… Australia!
Scary stuff. All this talk of us wearing our ADRs out, when there is a high probability they will outlast us!
UPDATE:
The incision hurt like heck until about the 4th day post-op. They did end up going pretty deep and wide on the re-excision just to be safe. The scar is a little bigger and WAY uglier than my ADR incision. It’s crazy that a tumour less than .80mm thick calls for an excision like this!
I wasn’t sure I should post this on my site, but I think it is very important for us ADR patients to think as far down the road as you can. I hadn’t really thought about the repercussions of ADR with any other life-threatening conditions years down the road, but I sure as hell did last week. It’s great to lessen our back pain, but can an artificial disc increase our likelihood of adverse reactions if ever immunosuppressed? This is an important question to address for peeps like us!
Feb 28th Update – I got the results back from my re-excision and the margins are all clear. My follow-ups are now only every 6 months for the next year or so. Thank god!
-Brett